Insomnia is perhaps, one of the most common sleep disorders known to us. It is known to affect up to 70 million Americans yearly, while its symptoms are experienced by 33%-50% of the adult US population. To an ordinary person, insomnia is the inability to fall asleep or remain asleep throughout the night. As a result of this, you may feel lethargic and less productive the next day. However, many people do not know the complexities of insomnia, including psychophysiological insomnia, and how each of us is at risk for it.
Insomnia – the inability to fall asleep!
What you know about insomnia is correct, but there’s more to it. It is a sleep disorder and is divided into two categories, based on its frequency and etiology.
When we talk about insomnia being differentiated based on frequency, we call it acute or chronic.
Acute insomnia is what most of us have experienced more than often, especially during stressful times. It is a short-term condition that may last from a few days to a few weeks. It is also known as adjustment insomnia because it manifests after someone experiences a stressful event.
Chronic insomnia:
Chronic insomnia, on the other hand, is said to exist when the symptoms persist for a minimum of three nights for a month or longer. This type of insomnia presents a long-term pattern of difficulty sleeping and is also associated with the risk of developing cardiovascular diseases, diabetes, and obesity.
Apart from the distinction between acute and chronic insomnia, sleep disorder is also classified according to its etiology into primary and secondary insomnia. Insomnia that does not occur due to an underlying condition is known as primary insomnia. However, its onset is influenced by various factors that may have a psychophysiological (i.e., both physical and mental) origin. Such factors include anxiety, stress, and even fear of not being able to sleep at night.
Insomnia, no matter which category it belongs to, needs timely medical assistance since it has the ability to perpetuate serious medical concerns. One such example is our topic of interest – psychophysiological insomnia, which belongs to the umbrella of both chronic and primary insomnia. It is a sleep disorder that persists frequently for a considerable number of nights (chronic insomnia) and is worsened by stress (primary insomnia). It is a serious health concern that takes a considerable toll on your physical and mental well-being. We will discuss it in detail here to help you understand the condition better and to deal with it accordingly.
What is Psychophysiological Insomnia?
In psychophysiological insomnia, a person is unable to sleep due to pronounced physical and cognitive arousal. This type of chronic insomnia stems from stress and manifests as a cycle. Someone who suffers from psychophysiological insomnia will tend to worry about their inability to sleep and how it would affect their productivity the next day. With time, this turns into a pattern, causing an increased state of stimulation, which further decreases the chances of initiating and maintaining sleep.
To sum it up, if you suffer from psychophysiological insomnia. You’ll worry about your sleep and it will further interfere with your ability to sleep. As a result, with each passing sleepless night, the condition worsens. In this way, it also resembles performance anxiety, in which a person fears their inability to perform a particular task.
The Onset of Psychophysiological Insomnia:
As previously discussed, the onset of this type of insomnia is contributed by stress. However, the psychological factor can be due to unplanned lifestyle modification, triggers of short-term stressors, and even poor sleep hygiene. People who are surrounded by loud noises or intake coffee and heavy meals before bedtime may struggle to fall asleep. Hence, with time, their habits may trigger the onset of sleep-onset insomnia.
Its Etiology and Pathophysiology:
While there is little to no information to elaborate on the etiology and pathophysiology of psychophysiology insomnia. However, with that being said, existing studies have shown the link between chronic and severe insomnia in characterizing this particular type.
How is Psychophysiological Insomnia Diagnosed?
In addition to not being able to sleep because of stress or anxiety, psychophysiological insomnia presents some other clinical symptoms. If you believe to be suffering from this disorder, read the following criteria and evaluate your sleep pattern:
- Insomnia that has continued for at least a month
- Insomnia is not related to any physical or mental health condition or any medication
- Struggling to fall asleep at a designated time but falling asleep when you do not intend to
- Struggling to fall asleep even in a feasible environment
- Poor sleep quality
- Feeling more alert at planned bedtimes
If you relate to any of the aforementioned conditions, we recommend you seek medical advice. Your physician will perform a physical exam to determine factors that affect your sleep. They will also ask you to monitor your sleep pattern and record it in a sleep diary for a better assessment of your sleep routine.
In some cases, physicians might also suggest a sleep study like polysomnography (in-clinic sleep study) or a home study test. These tests are diagnostic tools that leverage changes in physiological parameters such as brain waves, eye movement, and breathing rate to diagnose a sleep disorder.
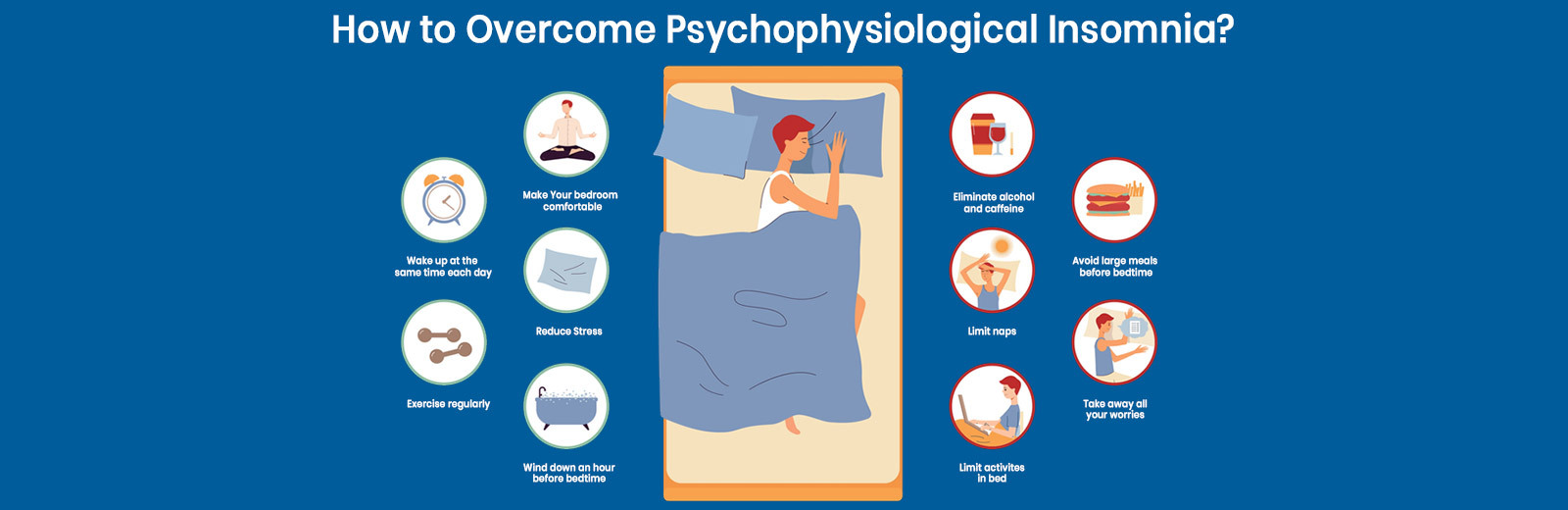
How to Overcome Psychophysiological Insomnia?
To overcome pathophysiological insomnia, you first need to understand it and its remedial approach. Since stress has already been playing a vital role in this condition you will worsen the disorder by fretting over its scope of treatment.
Therefore, the first step is to tell yourself that this is a manageable condition and that you can overcome it.
As we previously discussed, psychophysiological insomnia shares traits with performance anxiety. The latter is a condition in which one may become anxious about performing a task, such as appearing for an interview or performing on a stage. With this type of insomnia, the task is to sleep, which people struggle with. Moreover, they’re also concerned about its consequences and that is less alertness and productivity the next day. With time, the brain begins to interpret bedtime as a threat, and the person may experience pronounced physical and mental alertness.
However, just like those with stage fright can turn off the light and overcome their fear, those with psychophysiological insomnia can overpower their condition too. How? The answer lies below.
What are some Treatment Strategies?
While there is not a specific blueprint for the treatment of psychophysiological insomnia, physicians have derived a strategy from multiple options. These include medications, therapies, and lifestyle changes, all of which help in overcoming sleeplessness.
Pharmacological Approach:
The treatment of psychophysiological insomnia involves the use of four classes of drugs. These drugs may be used as per needed for short-term relief and also for long-term management. However, they also pose some adverse effects such as drowsiness during the day which can slowly become a habit. Hence, it is important to discuss these conditions with your physician for adequate guidance.
The first class of drugs used for the treatment of psychophysiological insomnia includes sedative hypnotics. Amongst which the efficacy of benzodiazepines and benzodiazepine receptor agonists is often compared. The second approach involves the use of melatonin agonists to stimulate the circadian cycle and manifest sleep. The third treatment option is to use low-dose doxepin as it has shown potential to reduce the risk for side effects and improve tolerance in elderly patients. Lastly, physicians also leverage antidepressants to reduce stress and anxiety. However, none of these classes of drugs are backed by limited data which renders physicians reluctant of using them. Hence, they are more inclined toward another treatment scheme, i.e., cognitive-behavioral therapy for insomnia (CBT-I).
Cognitive-Behavioral Therapy for Insomnia (CBT-I):
Cognitive-behavioral therapy for insomnia is termed the first-line treatment for psychophysiological insomnia. Unlike the drugs that induce sleep, the therapy focuses on the factors that affect your sleep It deals with analyzing a person’s thoughts, emotions, and behaviors that may manifest the onset of the specific sleep disorder.
CBT-I aims to help people realize their thought patterns. That damage the sleep pattern that prevents them from falling and remaining asleep. One of the purposes of the treatment is to empower the patient to address their resentment towards their inability to sleep and then have to bear its fruit at work the next day.
One of its approaches is to educate people about sleep hygiene and stimulus control and how by maintaining a proper schedule, people can get quality sleep.
Non-pharmacological Approach:
The non-pharmacological strategy deals with lifestyle modifications that contribute to better sleep hygiene. If you are diagnosed with psychophysiological insomnia, you’ll be advised to:
- minimize screen time before bed as it stimulates the brain to remain awake.
- limit naps in the afternoon as it makes it even more difficult to sleep at night
- and reduce caffeine and alcohol consumption as it disrupts sleep quality.
End Note:
Stress can do a lot of damage to the human body and psychophysiological insomnia is its prime example. Here, at Lung-N-Sleep, we’re dedicated to helping you battle insomnia, which along with stress, negatively affects your quality of life.