What is Mild Pulmonary Vascular Congestion?
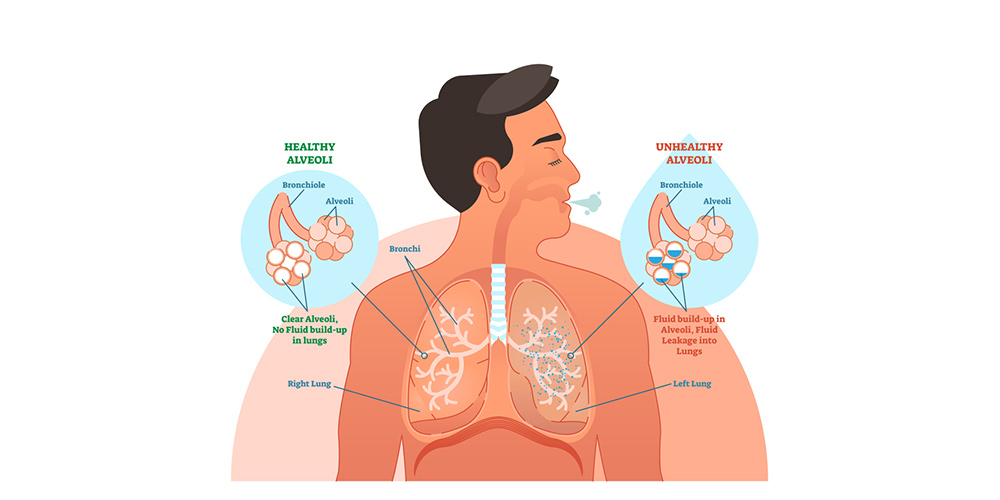
The enlargement of pulmonary blood vessels is called mild pulmonary vascular congestion or lung congestion. This condition is triggered when alveoli get filled with blood after blood vessels in the lungs distend, causing various complications.
Active VS Passive Pulmonary Congestion? What is the Difference?
Lung congestion is divided into active or passive congestion based on its etiology. The primary cause of active lung congestion includes infectious agents or irritants. Such substances cause the alveolar walls and their capillaries to distend with blood. On the other hand, passive congestion occurs due to high blood pressure in the capillaries present in the lungs. Hypertension, which leads to passive lung congestion, may be due to cardiac disorder or relaxation of capillaries which causes the blood to seep into the alveoli.
In bedridden patients, passive congestion occurs due to slightly different reasons. In such cases, the blood vessels relax due to weak cardiac activity. Eventually, blood concentrates in the lower part of the lungs, affecting some parts of the lung tissue. While a significant percentage of lungs remain unaffected and fit for respiration, complications like pneumonia can damage the remaining tissue.
What Causes Pulmonary Vascular Congestion?
Congestive heart failure is one of the leading causes of mild pulmonary vascular congestion.
In congestive cardiac failure, the left side of the heart is unable to pump blood to the general circulation. The heart is unable to evacuate the blood at the rate at which it receives blood from pulmonary circulation. Consequently, the pulmonary circulation experiences fluid backup and congestion, causing back pressure on the pulmonary vessels. Pulmonary vessels are responsible for delivering oxygenated blood to the heart. When the blood pressure increases in the alveolar capillaries, they swell. Eventually, the blood pressure gets too high, and blood leaks from the capillary walls into the alveoli, flooding them.
After the blood clogs the alveoli, the iron pigment in the blood seeps throughout the lungs. The metal then damages the lung tissues and leads to the buildup of scar tissue. As the disease progresses, the person may experience troubled breathing and bloody discharge and may also present skin with a bluish tint.
In some cases, a condition known as mitral stenosis also plays a part in the onset of chronic passive congestion. Mitral stenosis is described as the narrowing of the valve between the upper and lower chamber on the left side of the heart. Mild pulmonary vascular congestion in such cases is known as chronic passive congestion.
In addition to systolic left heart failure, other conditions account for mild pulmonary vascular congestion. For example, disorders that constrict pulmonary blood vessels and increase pulmonary vascular resistance also lead to the onset of lung congestion. Such conditions or disorders include:
- Inflammatory disorders.
- Autoimmune diseases.
- Intrinsic lung diseases.
- Bacterial infections.
- Structural defects.
- Drugs.
- Hypoxic conditions.
Pulmonary Congestion VS Pulmonary Edema
There are various types of pulmonary edema based on their precipitating cause. While inflammatory edema occurs due to influenza or pneumonia, mechanical edema results from decreased capillary permeability. The similarity between pulmonary edema and congestion is the cause that reduces capillary permeability, i.e., cardiac insufficiency and irritant particles. Furthermore, the edema also occurs after reinflation of a collapsed lung or post-operative surgery when a high volume of I/V fluids is administered.
Furthermore, like congestion, the edema also renders the person short of breath and the skin a bluish tint.
How to Identify the Onset of Pulmonary Vascular Congestion?
Physicians identify mild pulmonary vascular congestion through its characteristic signs and symptoms. The most common clinical presentation for lung congestion includes:
- Shortness of breath (SOB)
- Fatigue
- Peripheral edema (swelling in ankles, feet, and legs)
- Distended abdomen (swelling in the abdomen)
Some of the symptoms may aggravate after physical activity. For example, shortness of breath and fatigue may be more pronounced after routine physical exertion or climbing stairs.
The symptoms begin to get worse as the condition of the heart weakens. People with mild pulmonary vascular congestion may be out of breath even after getting dressed or walking a short distance. They also feel breathlessness while lying flat.
Since fluid buildup is a distinguishing characteristic of mild pulmonary vascular congestion, it also presents some signs and symptoms, such as:
- Weight gain.
- Frequent urination.
- Nocturnal cough that is worse while lying down.
The forenamed signs strongly indicate acute pulmonary edema and require immediate medical
The Diagnosis of Pulmonary Vascular Congestion
Physicians leverage physical and cardiac tests to diagnose mild pulmonary vascular congestion. The reason is that it is not possible to identify the condition through just one diagnostic test. By observing the patient’s signs and symptoms, physicians recommend various tests for a complete diagnosis.
Some of the diagnostic tests for mild pulmonary vascular congestion include:
EKG (Electrocardiogram):
The test monitors and records various cardiac functions. It determines cardiac electrical activity, how fast the heart beats, and whether it has a steady rhythm. Furthermore, EKG also registers the strength and frequency of electrical signals during their transmission through the heart. In addition, to determine cardiac functionality, EKG also monitors the heart’s physiological and anatomical features. For example, through EKG, physicians can deduce whether the pumping chambers are thicker than usual as thickened walls. By leveraging an electrocardiogram, physicians can also evaluate the signs of a previous heart attack or the onset of an active attack.
Chest X-Ray:
The diagnostic tool presents images of the chest and its structure, including the heart, lungs, and blood vessels. In case of mild pulmonary vascular congestion, physicians will observe a distended blood vessel or a part of the lung.
Brain natriuretic peptide (BNP) Blood Test:
The test measures the level of brain natriuretic peptide. This is a hormone that rises during cardiac arrest.
Echocardiography (echo):
Echo employs sound waves to generate a dynamic picture of the heart. The image then depicts the size and shape of the heart, its chambers, and its valves. Echo can detect areas that receive low blood flow and its damage. It also identifies the parts of the heart which do not contract ideally.
Doppler Ultrasound:
Like echo, doppler ultrasound also utilizes sound waves to determine the speed and direction of blood flow. Physicians recommend the test for better analysis of blood circulation to the heart and lungs and to identify the right-sided cardiac failure.
Holter Monitor:
It is a test that monitors cardiac electrical activity for a day or two while the person carries out their routine. The test requires electrodes in the form of small patches that connect to a portable recorder. You may wear the device and carry on with your day while it records the cardiac activity.
Nuclear Heart Scan:
The test also records the blood circulation and the speed and volume at which the blood reaches the cardiac muscles. It is an invasive test in which physicians inject a radioactive substance called a tracer, which travels to the heart and produces images on a camera outside the body.
Positron Emission Tomography (PET) Scan:
A PET scan is a type of nuclear heart that determines the extent of chemical activity in the cardiac regions. Physicians employ PET scans to see if any part of the heart is not receiving adequate blood flow.
Cardiac Catheterization:
It is an invasive test in which the physicians insert a long, thin, flexible tube into the body. The catheter provides images from inside the coronary arteries and reveals any blockage.
Coronary Angiography:
Coronary angiography usually runs simultaneously with cardiac catheterization. In angiography, a dye is put into the bloodstream via the catheter, which produces images on a screen. Physicians evaluate the scan to see how appropriately the heart is pumping blood.
Other diagnostic tests include a stress test, cardiac MRI, and thyroid function test. They determine cardiac function under stress, damaged areas of the heart, and the efficiency of the thyroid glands respectively.
Complications of Pulmonary Congestions – It’s Serious and Threatening
Mild pulmonary vascular congestion leads to two distinct phenomena,
- Pulmonary Arterial Hypertension, i.e., the blood pressure in pulmonary arteries (vessels that carry deoxygenated blood to the lungs) increases.
- Pulmonary Venous Hypertension, i.e., the blood pressure in pulmonary veins (vessels that carry oxygenated blood to the heart) increases.
Both pulmonary arterial and venous hypertension can manifest various diseases that belong to the umbrella term: Pulmonary vascular diseases. It includes;
- Chronic Thromboembolic Disease.
- Pulmonary Veno-occlusive Disease.
- Arteriovenous Malformations.
How is Pulmonary Vascular Congestion Treated?
The key to treating mild pulmonary vascular congestion is to look for its precipitating condition. Since congestive heart failure is the most prominent cause of mild pulmonary vascular congestion, physicians prefer its management first.
The treatment strategy includes;
- Reducing afterload (pressure that the heart resists while pumping) through antihypertensive drugs.
- Reducing fluid accumulation through diuretics to increase urine output.
- Amplifying pumping of blood through specific mediations.
- Treating other underlying conditions, such as pulmonary vasoconstrictions, through drugs that decrease resistance and congestion.
End Note
Mild pulmonary vascular congestion may not present prominent symptoms in its earliest stage but can progress into a fatal condition. You can keep a diligent eye on your cardiac and pulmonary health through regular checkups to ensure optimum health and well-being.
FAQs
What are the symptoms of pulmonary vascular congestion?
A number of symptoms are associated with pulmonary vascular congestion. Some may include:
- Fatigue.
- Shortness of breath.
- Fainting.
- Coughing up blood.
- Difficulty breathing normally.
As the disease gets worse, it causes swelling in the lungs, pulmonary hypertension, and different respiratory diseases.
How long can you live with pulmonary vascular congestion?
The survival rate for pulmonary vascular congestion depends on the severity of the condition. Some patients survive for 3 to 5 years after getting diagnosed, while others may only survive for about a year.
Is pulmonary edema the same as pulmonary vascular congestion?
Pulmonary edema is also known as pulmonary vascular congestion is the build-up of fluid in the tissue and air spaces in the lungs.
Does pulmonary vascular congestion mean heart failure?
Congestive heart failure is often the cause of pulmonary vascular congestion. When the heart does not pump blood efficiently it causes pressure in the blood vessels due to which fluid builds up in the air sacs.
Is pulmonary vascular congestion is serious?
It develops suddenly and should be treated immediately. If neglected, it can prove to be fatal. There are several deaths reported due to this condition.