Multifocal pneumonia is a respiratory infection that manifests in multiple areas within either one or both lungs. While viruses, bacteria, or fungi can be responsible for it, viral infections are the main cause.
Moreover, the symptoms associated with this condition are more intense compared to other pneumonia variations. The diagnostic procedures for it are similar to other types of pneumonia, and treatment typically involves a combination of rest, nutritional support, and medications tailored to address the specific causative agent.
What is Multifocal Pneumonia?
The lungs are a pair of respiratory organs that are divided into lobes. The right lung is large and has three lobes, while the left lung has two lobes. Moreover, air travels from the trachea to the bronchi into small air sacs known as alveoli. Additionally, alveoli are vital for oxygen exchange.
Pneumonia is a broad term indicating lung infection caused by inflammation, primarily affecting the lower lung regions, including the alveoli. Pneumonia is classified based on factors like the environment and the causative agent like bacterial, viral, or fungal influencing infection rates and severity.
Furthermore, it involves inflammation in multiple areas of lung lobes, potentially affecting one or both lungs.

Multifocal Pneumonia Cause
Pathogens (bacteria, viruses, and fungi) that cause other types of pneumonia also cause multifocal pneumonia. What characterizes this condition is how the disease presents in the lungs, with several sites of inflammation and infection. Below are the multiple Multifocal Pneumonia causes:
Bacterial Infections
- Streptococcus pneumoniae: This bacterium is a common cause of community-acquired pneumonia and can lead to this condition.
- Staphylococcus aureus: The bacterium causes various infections and can lead to this condition.
- Klebsiella pneumoniae: This bacterium is associated with healthcare-associated pneumonia. When the lungs are affected, it can cause inflammation in multiple areas.
Viral Infections
- Influenza viruses: These viruses are a common viral cause of pneumonia. This condition can occur when the virus infects different parts of the lungs and causes inflammation.
- Respiratory Syncytial Virus (RSV): RSV is a significant cause of respiratory infections, particularly in infants and older adults. When it causes pneumonia, it can spread to other parts leading to multifocal lungs. Similarly, it is common in children and adults.
- Adenoviruses: Is also known as COVID-19, cause respiratory infections that can lead to pneumonia with inflammation in the lungs.
Fungal Infections
- Aspergillus: It is a mold and can cause lung infections, particularly in individuals with compromised immune systems.
Non-Infectious Causes
- Aspiration Pneumonia: Caused by inhaling foreign material into the lungs. It can lead to inflammation in different areas, resulting in multifocal pneumonia.
- Chemical Pneumonitis: Exposure to irritating chemicals can cause inflammation in the lungs. Furthermore, if inflammation is widespread, it may contribute to multifocal pneumonia.
Autoimmune Conditions
- Rheumatoid Arthritis: Autoimmune diseases like rheumatoid arthritis can cause inflammation in the lungs.
- Systemic Lupus Erythematosus (SLE): It may involve the lungs and contribute to multifocal pneumonia due to widespread inflammation in the whole body.
Multifocal Pneumonia Symptoms
The symptoms are similar to other variations of pneumonia and can be either mild or severe. However, because of inflammation in different parts of the lungs, the infection can sometimes be severe enough to necessitate hospitalization.
The main symptoms of pneumonia can vary depending on the patient’s age and other circumstances. These include:
- Cough
- Fever
- Chills
- Shortness of breath
- Sputum production
- Chest pain if you breathe or cough
Multifocal Pneumonia Diagnosis
A thorough physical examination is the first step in the diagnosis of this condition. Clinical signs and symptoms are carefully evaluated by healthcare professionals, with an emphasis on respiratory indicators such as breath sounds, chest movement, and respiratory rate.
Moreover, doctors may prescribe you to take a blood test to figure out if there is any infection. Furthermore, sputum culture and analysis are critical in identifying the causal agent and directing the selection of the most efficient antibiotic or antifungal treatment.
Imaging Studies
Furthermore, healthcare professionals may perform imaging tests to accurately diagnose the condition.
-
Chest X-ray
Chest X-rays may swiftly diagnose lung damage by detecting areas of inflammation or consolidation. Multifocal pneumonia is a condition where there are multiple areas of infiltration or opacities present in different parts of the lungs.
-
Computed Tomography (CT) Scan
CT scans provide a thorough image of the lungs, which aids in determining the degree and distribution of inflammation. Moreover, patchy consolidations, ground-glass opacities, and nodules in various locations of the lungs are examples of CT scan abnormalities.
Bronchoscopy and Biopsy
In diagnosing infections, bronchoscopy proves invaluable as it identifies specific pathogens, assesses the presence of airway blockages, and offers crucial information to guide treatment decisions.
Similarly, a biopsy is taken to acquire a small tissue sample from the lungs for microscopic examination. Through microscopic analysis of the tissue sample, healthcare professionals can gain insights into the nature and extent of the infection.
Complications
Complications can occur following pneumonia in rare circumstances and if you have certain risk factors. Furthermore, some of these complications are as follows:
Acute Respiratory Distress Syndrome (ARDS):
In rare cases, individuals with pneumonia may develop Acute Respiratory Distress Syndrome (ARDS). ARDS is a serious and sometimes fatal syndrome caused by inflammation in the lungs. This results in decreased oxygen exchange. This condition can cause severe respiratory distress and might require advanced medical measures.
Sepsis:
Furthermore, the development of sepsis is a potentially fatal systemic response to infection. Sepsis is connected with bacterial pneumonia. It is the body’s severe response to an infection, resulting in extensive inflammation and probable organ failure.
Lung Abscesses:
It is defined by pockets of pus or fluid within or surrounding infected lung tissue. Lung abscesses can cause specific harm and can require specialized medical treatment, such as drainage techniques or focused antibiotic treatments.
Multifocal Pneumonia Treatment
The treatment plan will vary widely depending on the severity of the infection as well as the cause of pneumonia. Doctors might recommend a variety of therapy options like;
Antibiotic Therapy:
Antibiotic therapy involves the use of broad-spectrum antibiotics to target a range of potential bacterial pathogens. This is prescribed before specific information about the causative agent is available so that symptoms can be managed.
Targeted Therapy:
Once the causative agent is identified through diagnostic tests like sputum cultures or blood cultures. Antibiotic therapy can be customized to target the identified bacteria.
This targeted approach enhances the effectiveness of the treatment while minimizing the risk of antibiotic resistance.
Antiviral or Antifungal Medications:
Healthcare providers typically prescribe antiviral medications, such as oseltamivir for treating viral pneumonia. Additionally, the management of fungal pneumonia often involves administering antifungal drugs like fluconazole.
Ventilation and Hospitalization:
In rare situations, pneumonia can result in respiratory failure, in which the lungs are unable to supply enough oxygen to the body. Nevertheless, this severe condition may demand ventilatory support and critical care hospitalization. Prompt medical action is critical to maintaining respiratory function and improving recovery chances.
Oxygen Therapy:
It is essential when there is a significant decrease in blood oxygen levels. Hence, supplemental oxygen therapy is administered to support respiratory function and ensure proper oxygen supply to the body
Multifocal Pneumonia Mangement
-
Monitoring:
Monitoring and follow-up play a pivotal role in comprehensive management. Regular monitoring of clinical progress involves diligent physical examinations and imaging tests. Furthermore, follow-up is crucial for evaluating the effectiveness of the prescribed treatment, making necessary adjustments to medications, and promptly identifying any potential complications that may arise during the illness.
-
Preventive measures:
Preventive measures constitute an essential component of its management. Vaccination against common respiratory pathogens, including influenza and pneumococcal vaccines, serves as a proactive strategy to prevent pneumonia and its complications.
-
Multidisciplinary Approach:
When this condition is present as a complex condition, a multidisciplinary approach becomes vital to control the progression of the condition. Subsequently, collaborative efforts involving various medical specialists, such as pulmonologists, infectious disease specialists, and critical care physicians, allow for a comprehensive evaluation and optimization of patient care.
Case Study
A 13-year-old patient sought urgent medical attention at a hospital due to severe symptoms indicative of multifocal pneumonia. Upon arrival at the emergency department, the individual resented with acute hypoxemic respiratory distress, accompanied by a three-day history of persistent cough and worsening chest pain.
Despite the young patient leading a sedentary lifestyle without engagement in sports, there were no reported daily medications or environmental exposures. Additionally, there was no family history of pulmonary, autoimmune, or connective tissue diseases.
Consequently, to address the acute hypoxemic respiratory distress, the medical team started oxygen therapy as a supportive measure. However, it’s noteworthy that there is no treatment available for advanced infection. Management strategies can significantly impact outcomes when implemented at the right time.
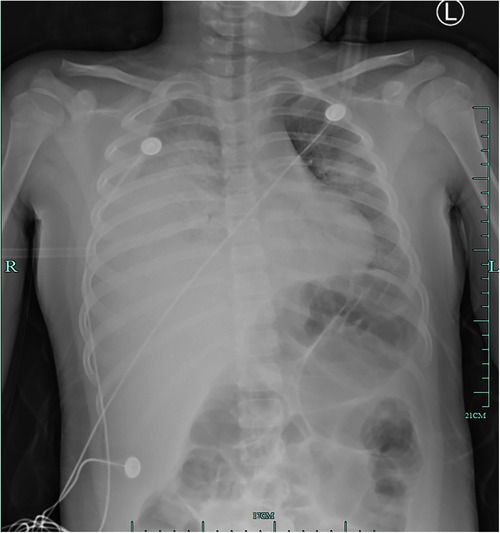
Figure: Multifocal consolidations and ground glass opacities are present, as are several small round lucent patches, most notably in the right middle lobe.
Conclusion
In conclusion, multifocal pneumonia demands a thorough and tailored approach to diagnosis and management. Early intervention, accurate identification of the causative agent, and timely initiation of treatment are pivotal for successful outcomes.
Furthermore, for personalized consultations with lung specialists, we encourage individuals experiencing respiratory symptoms or seek guidance at our clinics, where our expert medical team stands ready to provide expert care and support.