Introduction
The intricate network of the respiratory system, with its delicate balance and finely tuned mechanisms, is essential for sustaining human life. However, this system can exhibit various signs and symptoms when faced with challenges such as respiratory infections or underlying health conditions, including peribronchial cuffing or thickening. This comprehensive exploration will delve into the depths of peribronchial cuffing, unraveling its complexities, understanding its implications, and shedding light on the epidemiology and demographics associated with this phenomenon.
What is Peribronchial Cuffing?
Peribronchial thickening or cuffing is a radiological term that describes a specific pattern observed in chest imaging, particularly on chest X-rays or CT scans. It refers to the thickening of the bronchial walls, specifically the tiny airways that branch out from the central bronchi into the lungs. This thickening produces a characteristic appearance resembling a “cuff” around the bronchi, indicative of underlying pathology.
Pathophysiology of Peribronchial Thickening/Cuffing
However, it is crucial to delve into its pathophysiology to comprehend bronchial wall thickening entirely. This phenomenon typically arises due to inflammation and edema in the bronchial walls. The inflammation leads to an increased permeability of blood vessels, allowing fluid to accumulate in the surrounding tissues. In the context of peribronchial thickening, this fluid accumulation occurs around the bronchi, causing their walls to thicken.
Viral Pulmonary Infection: Results of CXR
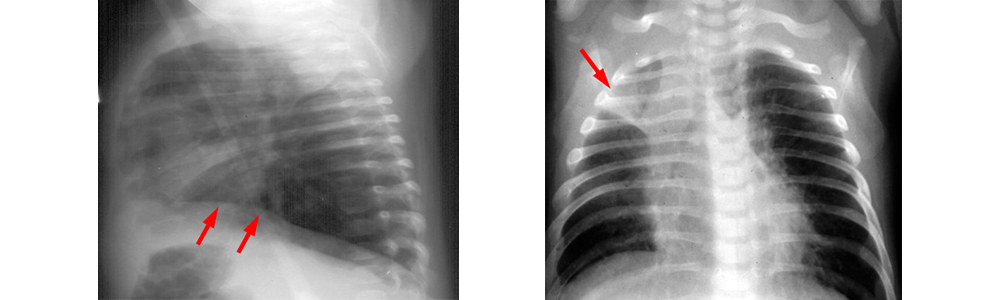
A peribronchial thickening or “peribronchial cuffing” on the CXR is a sign of bronchitis. However, a bronchus viewed endwise will exhibit thickening of the bronchial wall, and the lateral projection clearly shows the hilum’s unclean look.
Certain regions of the lung experience atelectasis and mucus plugging due to bronchial inflammation, while other areas show signs of hyperinflation from air trapping. Additionally, the diaphragms will flatten, and the anterior retrosternal gap will expand, resulting in an overall hyperinflated lung capacity.
Viral infections do not exhibit pleural effusions, but bacterial infections typically show this characteristic. However, the CXR results for viral infection and asthma, also known as reactive airway disease in preschoolers, are identical.
What Causes Peribronchial Cuffing?
Peribronchial thickening is often associated with various underlying respiratory issues; it is not a standalone condition. However, understanding these root causes is pivotal in comprehending the significance of peribronchial thickening in a clinical context. Some common causes include:
Pulmonary Edema:
Pulmonary edema, characterized by fluid accumulation in the lungs, can thicken the bronchial wall. The increased fluid in the lung tissue extends to the bronchial walls, causing them to concentrate nonetheless.
Respiratory Infections:
Infections such as pneumonia and bronchitis can trigger inflammation in the bronchial walls, resulting in peribronchial cuffing. The body’s immune response to pathogens can increase vascular permeability and subsequent fluid accumulation.
Allergic Reactions:
Allergic responses, particularly severe cases like anaphylaxis, can cause widespread inflammation, affecting and thickening the bronchial walls.
Heart Failure:
Congestive heart failure can result in the backup of blood into the pulmonary circulation, leading to increased pressure in the blood vessels. This elevated pressure can cause fluid to leak into the surrounding tissues, contributing to peribronchial thicking.
Autoimmune Disorders:
Certain autoimmune conditions, such as rheumatoid arthritis, may involve the respiratory system and lead to inflammation in the bronchial walls, manifesting as peribronchial cuffing.
Epidemiology and Demographics
Understanding the prevalence and demographics of peribronchial thickening is crucial for healthcare professionals, researchers, and patients. While specific statistics may vary based on geographic regions and populations, a general overview provides valuable insights.
Age Distribution:
Peribronchial cuffing can affect individuals of all age groups, from infants to older adults. However, specific causes, such as respiratory infections, may be more common in children, while conditions like heart failure may be more prevalent in older adults.
Gender Disparities:
Research indicates that peribronchial thickening does not exhibit significant gender-based variations. Both males and females can be equally susceptible to the conditions that give rise to this radiological finding.
Association with Pre-existing Conditions:
Certain underlying health conditions, such as chronic respiratory diseases, cardiovascular disorders, and autoimmune conditions, may predispose individuals to peribronchial thickening. Understanding these associations is crucial for targeted screening and management.
Geographic Variances:
Epidemiological studies have suggested that the prevalence of peribronchial thickening may vary across different regions. Environmental conditions, healthcare infrastructure, and population demographics can contribute to these variations.
Clinical Implications and Diagnostic Considerations
Peribronchial cuffing, as observed in imaging studies, is a valuable diagnostic clue for healthcare professionals. Recognizing this radiological sign prompts further investigation into the underlying causes, guiding appropriate therapeutic interventions. In a clinical setting, the following considerations are essential:
Differential Diagnosis:
Given that peribronchial thickening is a radiological manifestation, it is crucial to conduct a thorough differential diagnosis to identify the specific underlying condition. This may involve additional imaging studies, laboratory tests, and clinical assessments.
Peribronchial Cuffing Treatment Approaches:
The treatment of peribronchial thickening hinges on addressing the root cause. For instance, if the cuffing is a result of pulmonary edema, diuretics and interventions to manage heart failure may be indicated. In cases of infections, appropriate antimicrobial therapy is paramount.
Monitoring and Follow-up:
Regularly monitoring patients with peribronchial cuffing is vital to assess treatment response and identify potential complications. Follow-up imaging studies, pulmonary function tests, and clinical evaluations provide a comprehensive care plan.
Patient Education:
Educating patients about the underlying causes of peribronchia thickening, the importance of adherence to prescribed treatments, and lifestyle modifications can empower individuals to participate actively in their healthcare.
Peribronchial Cuffing Management
Addressing the underlying contribution to this radiological finding is inherently linked to managing peribronchial thickening. As peribronchial thickening is not a standalone medical issue but rather a manifestation of various respiratory and systemic disorders, the approach to management involves a thorough understanding of the root causes. Below is a comprehensive guide to the management of peribronchial thickening:
Identify and Treat the Underlying Cause:
The primary goal in managing peribronchial cuffing is to identify and address the specific condition or conditions leading to this radiological finding. Depending on the underlying cause, the treatment approach may vary. Common causes, such as pulmonary edema, respiratory infections, allergic reactions, heart failure, and autoimmune disorders, necessitate targeted therapies.
Pulmonary Edema Management:
In cases where peribronchial cuffing results from pulmonary edema, management involves addressing the fluid accumulation in the lungs. Diuretics, which promote the excretion of excess fluid through urine, are commonly prescribed. Additionally, treating the underlying cause of the edema, such as congestive heart failure or renal dysfunction, is crucial.
Antimicrobial Therapy for Infections:
If peribronchial thickening is associated with respiratory infections like pneumonia or bronchitis, appropriate antimicrobial therapy is essential. However, the choice of antibiotics depends on the suspected or identified pathogen. Early and targeted treatment also helps resolve the infection and reduces inflammation.
Anti-Inflammatory Medications:
Physicians may prescribe anti-inflammatory medications like corticosteroids if peribronchial cuffing is associated with inflammatory conditions such as autoimmune disorders or severe allergic reactions. These drugs help suppress the immune response and reduce inflammation in the bronchial walls.
For peribronchial thickening related to congestive heart function. Healthcare providers commonly prescribe medications like angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, and diuretics—lifestyle modifications, including dietary changes and regular essential treatments of heart failure management.
Bronchodilators and Respiratory Support:
Prescribing bronchodilators to alleviate airway constriction may be necessary in cases where peribronchial thickening is associated with chronic obstructive pulmonary disease (COPD). However, respiratory cases and respiratory support, including supplemental oxygen therapy in severe cases, may be necessary.
Monitoring and regularly monitoring patients with peribronchial thickening are critical to evaluating the treatment response and identifying potential complications. Moreover, follow-up imaging studies, pulmonary function tests, and clinical assessments provide a comprehensive care plan. However, healthcare professionals may adjust the treatment based on the patient’s progress.
Patient Education:
Educating patients about adhering to prescribed medications, lifestyle modifications, and regular follow-up appointments is integral to successful management. Inform patients promptly about potential triggers, exacerbation of peribronchial cuffing symptoms, and when to seek medical attention.
Addressing Underlying Risk Factors:
Managing peribronchial cuffing also involves addressing underlying risk factors, such as smoking cessation for individuals with chronic respiratory conditions or implementing measures to control allergic reactions. However, lifestyle modifications contribute to long-term management and prevention of recurrent episodes.
Collaborative and Multidisciplinary Care:
The management of peribronchial thickening often requires a collaborative and multidisciplinary approach. Additionally, pulmonologists, cardiologists, infectious disease specialists, and other healthcare professionals may collaborate to ensure comprehensive care and address the diverse aspects of the underlying conditions.
Conclusion
In conclusion, peribronchial cuffing represents a fascinating yet clinically significant radiological finding in respiratory health. Understanding its pathophysiology, common causes, and associated epidemiology provides a holistic perspective for healthcare professionals. Recognizing peribronchial thickening in imaging studies is a valuable tool in diagnosing and managing underlying respiratory conditions, ultimately contributing to improved patient outcomes and quality of life. As medical research advances, further insights into the complexities of peribronchial thickening may pave the way for more targeted interventions and enhanced patient care.